Music Therapy
Music Therapy-induced speech and communication in older adults
Abstract
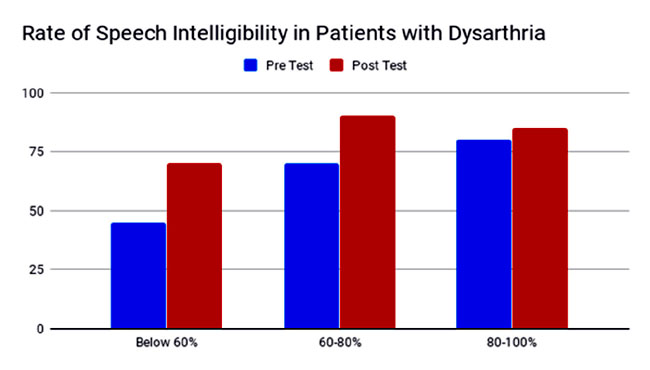
This research article investigates the effects of vocal exercises and singing on intelligibility and speech naturalness for subjects with acquired dysarthria due to Parkinson’s, traumatic brain injury, stroke, and neuro-degenerative diseases. A multiple case-study design was used, involving pre, mid, and post-treatment assessments of intelligibility, rate, and naturalness, on four subjects with dysarthria. Each subject participated in 60 weekly group music therapy sessions, involving Rhythmic Speech Cueing, and therapeutic singing techniques of neurological music therapy in combination with the traditional music of India which is based on Indian classical raagas.
Results were measured using a standardised dysarthric speech assessment — the Sentence Intelligibility Test and ratings of speech natural-ness. Statistically significant improvements in functional speech intelligibility were achieved with improvements in the rate of speech. The findings and conclusion of the research suggest that the music therapist designed a well-strutured music therapy programme with more than 50 weekly sessions on ‘metric cueing’ of vocal exercises and singing, which may faciitate more normative speech production for people with acquired dysarthria and support the need for further research in this area.
Definition
Dysarthria refers to a group of motor-speech impairments that result from damage to the neurological areas that control the muscles used for speech. Due to the underlying damage, the muscles of the tongue, lips and face do not respond in the normal way, and speech often becomes quiet, slurred, or unintelligible. These muscular deficits can affect the range, timing, speed, and steadiness of oral movement coordination.
According to the American Speech-Language-Hearing Association (1), dysarthria can affect one or more of the following five systems that speech involves:
• Respiration: respiration moves air across the vocal cords, creating sounds that the mouth and nose shape into words.
• Phonation: this system uses airflow from the lungs plus vocal cord vibrations to produce speech sounds.
• Resonance: resonance refers to the quality of speech sounds that the vocal tract produces.
• Articulation: this term means shaping sounds into recognisable words, which involves forming precise and accurate vowels and consonants.
• Prosody: the rhythm and intonation of speech that give words and phrases their meaning.
These five speech systems work together, meaning that impairment in one system can affect the others.
The American Music Therapy Association defines music therapy as the clinical and evidence-based use of music interventions to accomplish individualised goals within a therapeutic relationship by a credentialed professional who has completed an approved music therapy programme (2).
Music therapy interventions can be designed to:
• Promote wellness
• Manage stress
• Alleviate pain
• Express feelings
• Enhance memory
• Improve communication
• Promote physical rehabilitation
Neurologic music therapy (NMT) is a form of music therapy developed for people suffering from cognitive, sensory, or motor dysfunctions arising from neurological diseases of the nervous system. People who can benefit from this therapy include patients suffering from stroke, traumatic brain injury, Parkinson’s and Huntington’s diseases, cerebral palsy, Alzheimer’s disease, autism, and other neurological diseases affecting cognition, movement and communication.
In the Rhythmic Speech Cueing (RSC) technique, speech rate control via auditory rhythm is used to improve temporal characteristics such as fluency, articulatory rate, pause time, and intelligibility of speaking. Speech rate can be the primary therapeutic focus as in fluency disorders, or the tempo of speech can take on a mediating role for articulatory precision and thus speech intelligibility.
Therapeutic Singing (TS) refers to the more generalised use of singing activities for a variety of therapeutic purposes. Therapeutic singing allows direct engagement in musical creation. It can be a very success-oriented technique, thus providing important motivational input in tandem with functional enhancements to the client. This technique can synthesise a range of specific speech-language and respiratory control. (3)
Target population
In this research paper, the main clinical target population for induced speech and communication through music therapy is sufferers of acquired dysarthria. This is a neurological motor-speech impairment characterised by slow or hastened, weak, uncoordinated movements of the articulatory muscles. It results in reduced speech intelligibility and leads to communicative difficulties. The neurological damage underlying dysarthria may occur as a result of a stroke, traumatic brain injury or neurodegenerative disease.
Research
Beginning in the 1950s, music therapists, as well as other professionals in the area of speech and language rehabilitation, began to document case-studies and observations of the effectiveness of singing facilitating speech for people with aphasia, apraxia, language delays, and other speech disorders (4).
Michael Thaut and colleagues conducted an experimental trial on 20 patients with Parkinson’s disease who had mild to severe forms of dysarthria. They found a significant improvement among initially poorly intelligible participants (with the intelligibility of less than 60%). Cueing was most efficient at 60% of the habitual speaking rate. The best cueing modus was one syllable per beat. (5)
Pilon and colleagues conducted a study of three traumatic brain injury patients with mixed dysarthria. They compared RSC (metric cueing word by word at the reduced pacing rate of 80%) with singing at an equally reduced pace and the pacing board (a small board with five marked sections for the patients to tap with each word). In this small study, RSC caused the largest improvements in intelligibility. (6)
Tamplin conducted a pilot study to investigate the effect of vocal exercises on intelligibility and speech naturalness for people with dysarthria due to TBI or stroke. In individual music therapy sessions, a wide range of musical exercises, involving oral motor and respiratory exercises (OMREX), was applied. Some of their results, after 24 music therapy sessions, showed enhanced use of respiratory capacity and support, which was expressed by fewer pauses in the post-treatment speech. Due to improved respiratory capacity, the patients were also able to speak more words per phrase and showed more natural speech rhythms than before treatment. Tamplin also documented a carry-over effect that led to an increase in functional communication by some of the participants following the music therapy intervention. (7)
Therapeutic mechanisms
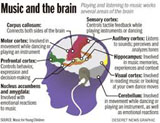
As speaking is a very complex sensorimotor function of numerous muscles, the rhythmic structure facilitates better coordination of the articulatory muscles. In that sense, the speech motor function shows the same sensitivity to rhythmic entrainment as can be seen in gross or fine motor functions. In other words, the acoustic rhythm seems to facilitate better motor programming in the process of speaking. This certainly holds true for all forms of dysarthria in which muscle functions are impaired. Considering the therapeutic mechanisms for RSC in dysarthria slowing down is clearly the main impact in terms of functional gains in intelligibility.
Van der Merwe states that musical exercises in which speech movement patterns are mimicked or practised are more likely to cause the neural adaptation necessary to improve speech precision than in simple resistance exercises focused on building oral muscle strength. Both speech and singing involve the use of muscles of respiration and articulation and contain elements of rhythm, pitch, dynamics, tempo, and diction. It is not surprising then, that speech and singing share many of the same neural mechanisms, which can influence each other in a therapeutic process. In singing, the word production rate is slower than in spoken language, and rhythmic and melodic speech inflections are more pronounced. While singing, a clear rhythmic cue is provided from the song that helps to stimulate and organise the motor function of the oral muscles. This rhythmic cue is especially strong while singing single syllables or sounds, and supplies an organised and highly repetitive frame through the song presentation. Special singing exercises can be used that support and shape oral fine motor skills in order to enhance coordination of the lips, tongue, and movements of the jaw. Such improvement can result in better articulation and intelligibility of dysarthric speech (8).
Therapy procedure
1. Diagnosis and clinical assessment
Before starting the music therapy sessions, it is essential to define the speech pathology. When assessing the speech problem, three questions need to be addressed:
• Is it a form of altered speech due to a neurological disease?
• Does the altered speech pattern cause any objective or subjective problem for the patient?
• Does the prognosis of the symptom justify initiating therapy?
If all three questions are answered in the affirmative, the patient should be referred for therapy.
2. Developing the clinical goal/objective
Once the speech pathology has been thoroughly described, the second step consists of the development of appropriate and measurable therapy goals and objectives. So in this step, according to the findings of the assessment, we define a clear and realistic aim like 1) improve intelligibility; 2) sharpness of articulation; and 3) speech fluency
3. Design of functional, non-musical therapeutic exercise
This step consists of the design of therapeutic exercises, structures, or therapeutic stimuli to accomplish the clinical objective. To assess the natural speech rate and/or fluency of a patient is to record their free and consecutive speaking for one minute and then count the syllables while listening to the recording.
4. Functional therapeutic musical exercises
In this step, the professional music therapist is using the tools and techniques of neurologic music therapy and translating functional and therapeutic exercises, and stimuli into functional therapeutic music exercises and stimuli. Speech pacing in dysarthria rehabilitation is accomplished through rhythmic cues in musical stimuli. The therapist can apply a combination of Rhythmic Speech cueing followed by Therapeutic Singing for better results.
5. Reassessment
In this step, music therapists reassess the patient’s progress using the same assessment tool from Step 1 to be able to compare and benchmark the effectiveness of treatment. Reassessment may occur during the treatment process, and at the end of treatment and at follow-ups.
6. Transfer of therapeutic learning to functional applications
Step 6 deals with transfer exercise from treatment training to activities of daily living. One of the main underlying principles in therapeutic training to recover functions or learn new functions is based on neuroplasticity — that is, the ability of the brain to reorganise or rewire itself to build new neural connections (9).
Clinical application
Skill area targeted: speech intelligibility, rate, and naturalness.
Age group: 4 subjects aged 65 to 80 years Setting: individual music therapy sessions.
Clinical diagnosis: dystharia due to Parkinson’s, traumatic brain injury and neurogenetic disorder.
Music Therapy techniques: a combination of Rhythm speech cueing (RSC) and Therapeutic Singing (TS).
Number of sessions: 60 weekly sessions.
A systematic step-by-step training scheme is developed to transfer the therapeutic musical exercises to functional activities of daily life. This is derived from an evidence-based hierarchical training scheme and it builds up from cued reading to free speaking in every session (10).
1. Out of the 20 older adults from the regular music therapy group, four had been chosen based on the assessment of speech intelligibility, rate, and naturalness, for specific individual music therapy training schemes for subjects with dysarthria to induce speech and communication skills.
2. After the selection process, the music therapist needs to test the patient’s rhythmic entrainment ability. Here the patient should be asked to follow a comfortably paced beat with the hand. This could be done with an electronic tabla app/metronome set to 100 bpm. In the next step, the tempo and mode of stimulation need to be defined.
3. In this step, the simple mode of stimulation is metric cueing, in which each syllable is matched to one beat from the metronome. We used Raag Yamen to sing and try to develop the oral-motor coordination and practise one syllable per beat.
Swara Rhythm — Sa Ni Dha Pa Ma Pa Ga Ma Pa Pa Re Ga Ni Re Sa
Spoken Rhythm — Pa Ya Li Ya A A MoRi Ba Je Re Pi ii Ya A
Rhythmic Stimulation — xxxxxxxxxxxxxxx
4. In this step, the patient is asked to read in the defined tempo and mode text material that is optimally structured for their speaking ability with a metronome and try to speak one syllable per beat in a slow and fast pace. The patient should speak freely to rhythmic stimulation.This usually works best when the therapist is asking very simple questions (What is the day today?; What did you have for breakfast?; etc.) The therapist is given a monologue on a chosen topic. This step was the most important in the RSC training and took maximum time than the other training steps in the session.
Swara Rhythm — Sa Re Ga Sa Re Ga
Spoken Rhythm — What is the day today
Rhythmic Stimulation — xxxxxx
5. In the final step the patient is asked to speak freely without rhythmic stimulation, but maintaining the objectives of therapeutic goals and the therapist suggested some transfer exercise to be carried out after therapy.
Swara Rhythm — Sa Re Ga Re Ga Ma Ga Ma Pa Sa (Pause)
Spoken Rhythm — went for a ride in a green-coloured shoe (pause). Now is the time that we find what to do (pause)
Conclusion
The findings and conclusion of this research article provide an evidence-based view of Music Therapy on effective, appropriate and specific treatment techniques for improving the quality of speech production and communication in older adults. The research has been focused on high prevalence speech pathology, such as acquired dysarthria.
1. The improvement of intelligibility, rate, and naturalness of the speech.
2. With the help of a well designed structural treatment plan by Music Therapist.
3. The treatment plan is structured and equipped with the combination of neurological Music Therapy Techniques, i.e. Rhythmic Speech Cueing (metric cueing) and Therapeutic Singing and traditional Indian Classical Music.
4. Assessments and Re-assessments of subjects during the 65 weekly sessions are the key components of the evidence-based research.
References
1. American Speech-Language-Hearing Association [Online] Available from:
https://www.asha.org/PRPSpecificTopic.aspx?folderid=8589943481§ion=Signs_and_Symptoms [Accessed 17th August 2020].
2. American Music Therapy Association [Online] https://www.musictherapy.org
3. Thaut MH, Hoemberg V. (2014), Handbook of Neurologic Music Therapy. Oxford University Press; 2014, pp.150-95.
4. Cohen NS. Speech and song: implications for music therapy. Music Therapy Perspectives, Oxford Academic1994; 12(1),:8-14.https://doi.org/10.1093/mtp/12.1.8
5. ThautMH, McIntosh KW, McIntosh GC, Hoemberg V. (2001). Auditory rhythmicity enhances movement and speech motor control in patients with Parkinson’s disease. Functional Neurology 2001; Henrich Hen University Dusseldorf Germany 16: 163-72.
6. Pilon M A, McIntosh KW, Thaut MH. Auditory vs visual speech timing cues as external rate control to enhance verbal intelligibility in mixed spastic dysarthric speakers: a pilot study. Brain Injury 1998; 12: 793-803 PMID: 9755370. DOI: 10.1080/026990598122188.
7. Tamplin J. (2008). A pilot study into the effect of vocal exercise and singing on dysarthric speech. NeuroRehabilitation 2008; 23: 207-16.PMID: 18560137.
8. Van der Merwe A. A theoretical framework for the characterization of pathological speech sensorimotor control. Clinical Management of Sensorimotor Speech Disorders. New York: Thieme Medical Publishers Inc.; 1997, pp.93-95.
9. Thaut MH.. Rhythm, Music, and the Brain: scientific foundations and clinical applications. New York: Routledge; 2005.
10. Ramig LO, Sapir S, Fox C, Countryman S. (2001).Changes in vocal loudness following intensive voice treatment (LSVT) in individuals with Parkinson’s disease: a comparison with untreated patients and normal age-matched controls. Movement Disorders 2001;16: 79-83.
Aradhana Deogharia is a neurological music therapist and the Founder and President of NAVYA Foundation, USA.
Share with us (Comments,contributions,opinions)
When reproducing this feature, please credit NAMAH,and give the byline. Please send us cuttings.