Mental health
Cultural U-turns in understanding mental health
Abstract
This article explores systematic cultural U-turns which occur globally, and it suggests we are heading towards another change regarding our understanding of consciousness and mental well-being. It also presents older assumptions around mental well-being, and newer ways of understanding and addressing human experiences.
Introduction
What is a cultural U-turn? In the past we (society) accepted certain kinds of knowledge as ‘truth’. Our governments made laws, which criminalised certain groups of people, who decades later were better understood. Governments then changed their minds about what was correct, revoked laws and apologised for their earlier actions.
Our beliefs about mental health are culturally determined. Today there is a gap between the beliefs of some physicians and some patients, and the aim of this article is to address a gap in understanding, explore some ancient wisdoms and suggest that it is time for another cultural U-turn in understanding.
Today many people support a new paradigm of consciousness, which embraces anomalous, extreme, clairvoyant and spiritual experiences. They question the pathology around intense experiences and consider it time to call a halt to the out-dated Eurocentric disease-model of human suffering, and to raise awareness of cultural ways of interpreting ‘symptoms’, in order to benefit the mental well-being of global populations.
Overview
In the first part of this article, I have summarised old-fashioned assumptions around mental health, the treatment options and the dissemination about so-called evidence. The older assumptions, which included chemical imbalance, disease of the brain, ethnic predispositions and illness for life, resulted in stigma and discrimination. I have noted that from within the profession, anti-psychiatry and critical psychiatry movements developed, which questioned evidence and research data.
In the second part, I present the new terminology for intense experiences and the transitional use of old pathology labels. Mental health and spiritual experiences are on a continuum, and I have acknowledged trauma triggers and new treatment options. I have explored potential evidence about a normal range of altered states of consciousness, achieved spontaneously and by specialists. I end by suggesting a variety of ways forward, which acknowledge new paradigm thinking for societal benefit.
Old-fashioned assumptions
As more psychiatrists become aware of ethical dilemmas facing their profession, they emphasise the importance of social context for understanding distress, rather than biological origins. Evidence against old-fashioned psychiatry and reductionist Western medicine is growing from within the profession, and general physicians, psychiatrists and psychologists are seeking new ways of understanding.
Challenges are being raised which question biological causes of ‘mental illness’ in the Diagnostic and Statistical Manual (DSM), the theory of chemical imbalances and the efficacy and benefits of medication. The British psychiatrist, Moncrieff questioned whether psychiatric drugs targeted underlying diseases and she claimed drugs did not correct chemical imbalances (1). The social anthropologist, James Davies showed how scientific research was manipulated. He interviewed the originators of the DSM and discovered that it was created by discussion and without reference to scientific evidence (2).
In the USA, others investigated how pharmaceutical companies had corrupted the American Psychiatric Association and documented how the American public were misled about the biology of mental disorders, the validity of diagnoses, and the efficacy of psychiatric drugs (3). In late 2016, a conference was held in Gothenburg, Sweden on the risks and alternatives to pharmaceuticals (4), where speakers included psychiatrists and psychologists.
The problem lies within the education system in medical schools, whereby students are taught about the biological origin of mental diseases in the brain and the pharmaceutical drugs used to treat them. They learn about the predispositions of different ethnic groups towards psychosis (in a rather racist educational system). This teaching also ignores patients’ psycho-social histories of trauma, oppression, repression and suppression. In those days diagnosis depended on the beliefs of the observer (5, 6).
In some parts of the West, the practice of medicine does not require any knowledge of religion or spirituality. Apart from general physicians, specialist medical doctors focus on increasingly narrow aspects of the body. Furthermore, cultural blindness may exist, whereby professionals may believe cultural differences are of little importance, and view everyone through Western spectacles.
The new ways
In the West, several groups of people have expressed dissatisfaction with the current model of mental health diagnosis and treatment. These are:
• culturally new migrants, refugees and asylum seekers
• patients and carers who experience the mental health system
• psychiatrists who know their training doesn’t fit the spirit of the times
• psychologists aware of the importance of personal history.
In addition, there are the original peoples of Australia, Canada and USA who want their spirituality acknowledged, and do not want their spiritual practices pathologised. My aim is to acknowledge the dilemma between these different frameworks of knowledge and bridge the gap between the perspectives of physicians and those of their patients.
In this age of the Internet everything is seen, nothing can be hidden. If the mainstream press doesn’t cover a story, we find it mentioned on social media. If peer-reviewed journals avoid certain research topics, then social media will publish it. So our mainstream media appears to be playing ‘catch-up’.
Below I present a range of ways on interpreting human experiences, which when taken together provides evidence of narratives about altered states of consciousness.
Beliefs about survival beyond death and mental health
Many people believe an individual does not die with the body. They believe ancestors exert an influence over the living, and discarnate beings like djinns influence mental health. A human being is said to consist of physical and non-physical components, some of which precede and survive death. Belief in ghosts is ubiquitous in Asia and Africa. A person’s body is said to be permeable to ghosts and spirits of the dead, who could cause misfortune.
In the West, one part of the population believes there is only mundane physicality and no survival beyond death, while those who claim to be psychics, mediums or clairvoyants assert consciousness survives beyond bodily death. Is it possible that our understanding of physical reality and consciousness beyond death influences our interpretation of mental health symptoms?
Cross-cultural beliefs of survival beyond death
In the past there was an assumption that reincarnation beliefs were only held by Hindus. However, the American anthropologist, Obeyesekere argued that belief in reincarnation was also central to Native Americans, Africans and Oceanic peoples (7). Other anthropologists suggested Western scholars could not accept this, and so they neglected the study of it (8).
The psychiatrist, Stevenson claimed birth-marks were suggestive of survival beyond death. He suggested some kind of memory was transmitted between lives, and proposed reincarnation as the most suitable explanation (9). Young and Goulet suggested scholars rarely acknowledged as veridical, beliefs which were different from their own (10).
It is our beliefs which influence the ways we interpret and treat mental distress and extreme experiences. Evidence for survival beyond death comes from end-of-life experiences (11), bereavement visions (12), or from the memories of patients with organ transplants (13).
Inter-generational transmission of trauma
Epigenetics is the study of body cells influenced by external or environmental factors (beyond the genes). The theory of epigenetic inheritance suggests, for example, that the Nazi holocaust trauma in one generation passes on to the next generation, through the genes. “Genetic changes stemming from the trauma suffered by Holocaust survivors are capable of being passed on to their children, the clearest sign yet that one person’s life experience can affect subsequent generations (14)”. Post-Traumatic Stress Disorder (PTSD) and Trauma could occur across generations, to the children of people who had direct experience (15, 16).
Then there were those, who had Holocaust memories which came from another’s existence, and these included Shahar (17), Wardle (18), and Gershom (19). I am interested, as I too had memories from beyond birth, but not as far as I am aware, from my ancestral line.
Implications of survival beliefs
Is it possible that those with mental distress or extreme experiences are triggered not only by trauma from their current human existence, but also from one or more previous incarnations? Perhaps sufferers are sensitive to a previous scenario, or have developed PTSD from a remote memory? Is this possible? Indian psychiatrists suggest that influences on mental well-being may go beyond birth and childhood and include past lives and karma (20).
This material on ‘memories’ invites me to question the ‘diseases of the brain’ model of mental ill-health, alongside the evidence of Whittaker (21) and Davies (22). It illustrates how important it is for patients to explore their narratives in non-judgmental company. In the West, is it because we are not sure about what happens after death, that we become confused about psychosis, and near-death experiences? Although some people accept consciousness after death, many may have problems with non-corporeal discarnate entities with personality, except perhaps some Africans (23).
What is or is not mental health?
The question as to what is or is not a mental health problem is extremely contentious. This depends on the ways people interpret their symptoms or their conditions (even the word ‘symptom’ is value laden).
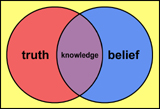
Let us explore assumptions around the terms ’knowledge’ and ‘belief’. We need to consider many perspectives for healthcare in our multi-cultural societies. In the past we became accustomed to an ‘us and them’ approach (24): that is we (Westerners) had ‘knowledge’ (correct explanation) whereas they (others) had ‘beliefs’ (which were erroneous).
Although it is clear what is and is not a mental health problem, in practice, we become concerned when people cannot stop the experience at will, or do not have the relevant framework of understanding.
Is it possible that people experiencing mental distress episodes are having spiritual experiences, but cannot switch them off? If they become hyper-sensitive or confused by being caught up in visions, surely this would result in anxiety or distress?
Unusual experiences
My proposition is that some people who spontaneously have NDE, OBE, ELE experiences (religious experiences; near-death, out-of-body, and end-of-life experiences) may not have a framework for understanding them, and in association with other factors, may attract psychiatric attention. I suggest some people who have extreme experiences, may be experiencing an NDE, OBE or ELE together with anxiety and distress.
In addition, there are some specialists like shamans and psychics who deliberately invite experiences and turn them on and off at will. Others have spontaneous experiences which stop. People who cannot control their experiences may come to the attention of psychiatrists. The phenomenology appears to be the same, although the effects are different. Is it possible that the human self is porous and, like a radio transmitter can change frequency, tune into different time and space frameworks? When we deny consciousness continuing after bodily death, perhaps we believe our own culture-bound explanations for mental suffering?
Opening the doors of perception
The data here is suggestive that anyone can open the doors of perception, while some people are born with the doors of perception open. I assume that all human beings have a normal in-built capacity to have ‘anomalous’ experiences, if not during their life, then at the end of their life.
Deliberate action to open perception
If visionary experiences are deliberately invoked, like those of writer, Joseph Rael (25), are they true or hallucinatory? How do they compare with someone who suffers a psychosis event? Most societies have specialists who are clairvoyant, psychic, shamans or mediums and can see into dimensions beyond, and who bridge realms of consciousness between health, life and death. These specialists deliberately move their centre of perception beyond the body into a non-local centre.
Is it possible people from indigenous communities have a greater awareness of subtle states of consciousness? In the old days, this was perhaps considered as ‘superstitious’, but today may be seen as having deep insight into altered states of consciousness. Perhaps Western society is wrong in its diagnosis of schizophrenia?
Remote-viewing
The topic of remote-viewing is contentious: military organisations in various countries deny being involved with it, and deny its efficacy (26). But I wonder, if remote-viewing can occur, is it possible that people having extreme experiences, are tuning into information from other places, like a radio? If they do not have a framework for understanding, would they not become anxious and confused? What is normal to one set of people may be considered abnormal to another.
Uprising of anger
Paranormal experiences, religious experiences and the symptoms of schizophrenia appear to lie at the ends of a continuum (27). People having anomalous experiences tap into a non-local realm and problems arise when this doesn’t fit in with their own or their observer’s belief systems. However, with social media more people are explicit about their experiences and the triggers for them.
Today social media offers evidence of an uprising of anger against Western psychiatry. Psychiatrists themselves are questioning such diagnoses (28, 29). Extreme experiences may also be called ‘Spiritual Crisis’ or ‘Spiritual Emergency’. Some people are sensitive and can access visionary experiences without taking any substances. Then there are people who have spontaneous experiences and are diagnosed as ‘schizophrenic’ by those who are not familiar with spiritual frameworks of understanding.
The new way forward seems to be present with suffering, rather than avoid it. People who did the new Open Dialogue and Peer-Supported Open Dialogue courses1 had dilemmas once they returned to work, where it was business as usual with their colleagues.
Cultural understanding
In the West, for years the dominant model of knowledge was biomedical and scholars mistakenly assumed it was globally ubiquitous. Now we understand a spiritual dimension exists, which some people access deliberately, some by chance, while others are disturbed and have no conceptual framework for understanding their experience. Each interpretation depends on common consensus of peers or colleagues. Today a turning-point is reached as we acknowledge deeper existential realities about being human.
Now for a full cultural U-turn we need to enhance education in our medical and healthcare establishments. My latest book, Cultural Perceptions on Mental Well Being (30) was written for medical and therapeutic practitioners to raise awareness of cultural and spiritual ways of interpreting symptoms. I hope it is used widely as a resource for front-line healthcare practitioners.
References
1. Moncrieff J. The Myth of the Chemical Cure: A Critique of Psychiatric Drug Treatment. London: Palgrave Macmillan; 2009.
2. Davies J. Cracked: Why Psychiatry is doing more harm than good. London: Icon Books; 2014.
3. Whitaker R, Cosgrove L. Psychiatry under the Influence, Institutional Corruption, Social Injury, and Prescriptions for Reform. New York: Palgrave Macmillan US; 2015.
4. Scientific symposium. [Online] http://extendedroom.org/en/scientific-symposium/ [Accessed 28th October 2016].
5. Tobert N. [Online], Human Experiences in Academic Boxes http://www.madinamerica.com/2015/01/human-experiences-academic-boxes/ [Accessed 28th October 2016].
6. Tobert N. Knowledge frameworks in medicine and health. NAMAH 2015; 23(3):8-14.
7. Obeyesekere G. Medusa’s Hair: An Essay of Personal Symbols and Religious Experience. Chicago: University of Chicago Press; 1981.
8. Mills A, Slobodin R. Amerindian Rebirth: Reincarnation Belief Among North American Indians And Inuit. Toronto: University of Toronto Press, 1994.
9. Stevenson I. Where Reincarnation and Biology Intersect. Westport, Connecticut, and London: Praeger; 1997.
10. Young DE, Goulet JG. Being Changed: The Anthropology of Extraordinary Experience. Toronto: University of Toronto Press; 1994.
11. Fenwick P, Fenwick E. The Art of Dying. London: Continuum; 2008.
12. Dewi Rees W. The Hallucinations of Widowhood., Br Med J 1971; 4:37.
13. Pearsall P. The Heart’s Code. London: Thorsons; 1998.
14. Thomson H. Study of Holocaust survivors finds trauma passed on to children’s genes, The Guardian, 21st August 2015.
15. Yehuda R, Golier J, Kaufman S. Circadian rhythm of salivary cortisol in Holocaust Survivors with and without PTSD. American Journal of Psychiatry 2005; 162: 998-1000.
16. Yehuda R. [Online] How Trauma and Resilience cross Generations (2015). Available at www.youtube.com/watch?v=LXgZamuTe3Q [Accessed 8th April 2016].
17. Shahar Y. A Damaged Mirror: A story of memory and redemption. Israel: Kasva Press; 2014.
18. Wardle E. ‘Death in the Consulting Room: Memories of the Holocaust and Questions of Past Lives’, MA Thesis (Distinction) 2014.
19. Gershom Y. Beyond the Ashes: Cases of Reincarnation from the Holocaust and from Ashes to Healing: Mystical encounters with the Holocaust. Virginia, USA: ARE Press; 1992.
20. Tobert N. Spiritual Psychiatries: Mental Health Practices in India and UK. Charlottesville, Virginia Create Space; 2014.
21. Whitaker R. Anatomy of an Epidemic. New York: Crown; 2010.
22. Davies J. Cracked: Why Psychiatry is doing more harm than good. London: Icon Books; 2014.
23. Adofo DY. Ancestral Voices: Spirit is Eternal. Charlottesville, Virginia: Create Space; 2016.
24. Good B. Medicine, Rationality and Experience: An Anthropological Perspective. Cambridge: Cambridge University Press; 1994.
25. Rael J. Being and Vibration: Entering the New World. San Francisco: Millichap Books; 2015.
26. Morehouse D. Psychic Warrior: True Story of the CIA’s Paranormal Espionage Programme. West Sussex, UK: Clairview Books; 2000.
27. Clarke I. Psychosis and Spirituality: Consolidating the New Paradigm. West Sussex, UK: Wiley; 2010.
28. Razzaque R. Breaking Down is Waking Up: Can Psychological Suffering be a Spiritual Gateway? London: Watkins Publishing; 2014.
29. Stockmann T. The UK National Health Service Peer-Supported Open Dialogue Project, Mad in America Blog. [Online]. https://www.madinamerica.com/2015/10/the-uk-national-health-service-peer-supported-open-dialogue-project/ (2015) [Accessed 8th February, 2016].
30. Tobert N. Cultural Perceptions on Mental Wellbeing: Spiritual Interpretations of Symptoms in Medical Practice. London: Jessica Kingsley Publishers; 2016.
1 Open Dialogue and Peer-Supported Open Dialogue are new ways of working in the UK National Health Service for people with first onset psychosis. Using group discussion with consent, the practice has taken off throughout Western countries. For millennia, it was a normal practice in African countries for addressing distress by a council of elders.
Dr. Natalie Tobert is a medical anthropologist based in the United Kingdom.
Share with us (Comments,contributions,opinions)
When reproducing this feature, please credit NAMAH,and give the byline. Please send us cuttings.